Tube feeding education
Types of Feeding Tubes and Methods of Feeding

There are several different locations, or routes, through which a feeding tube is placed to deliver the formula. Each of these routes allows the nutrients in the formula to be used by your body just as if you were eating a regular meal.
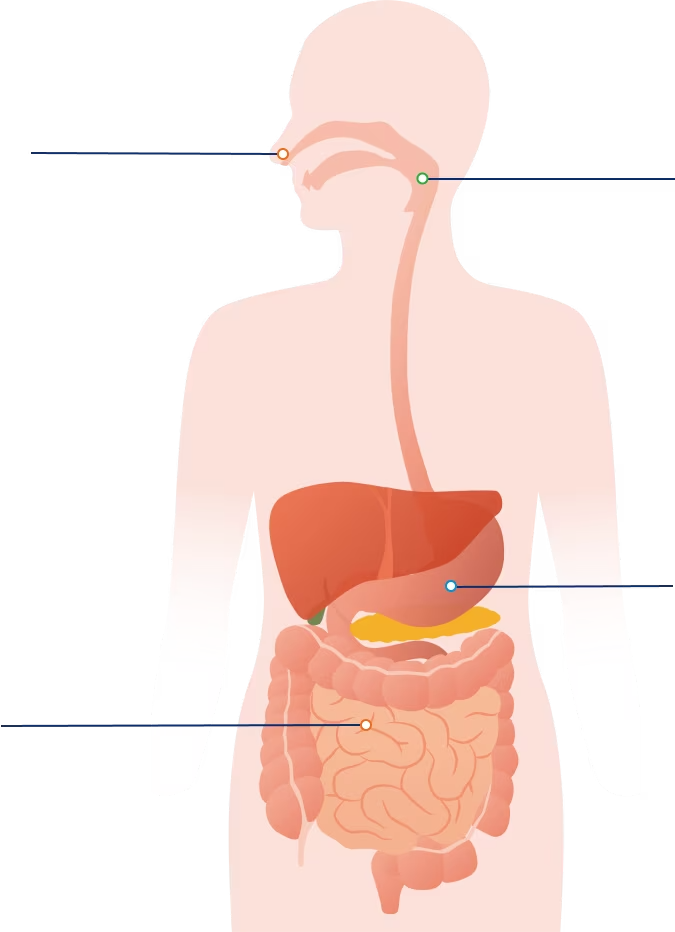
- Nasogastric or (NG-Tube). The feeding tube passes through the nose, down the throat and esophagus, and ends in the stomach.
- Nasointestinal (may be referred to as nasoduodenal or nasojejunal). The feeding tube passes through the nose, throat and esophagus, continues through the stomach, and ends in the first section of the small intestine.
- Gastrostomy (G-Tube). The feeding tube is inserted through the skin directly into the stomach.
- Jejunostomy (J-Tube). The feeding tube is surgically inserted into the jejunum — the middle section of the small intestine.
- Gastrojejunostomy (GJ-Tube). The feeding tube is surgically inserted into the stomach but will feed into the jejunum. The “G” portion can be used to vent, drain, or suction the stomach and the “J” portion can be used for feeding.
Your healthcare team has chosen the tube they believe will work best for you at home to make sure you receive the nutrition you need.
There are different ways to provide a tube feeding
Tube feedings may be:
- Bolus or Intermittent: formula is given at mealtimes or spread out during the day at specific times For example, feed at 8 am, noon, 6 pm or every four to 6 hours.
- Continuous: formula is delivered all day or for many hours throughout the day and/or night typically delivered by a feeding pump.
- A mix of these two methods
Depending on the tube feeding plan, the formula may be delivered by:
- Syringe (for bolus feeding).
- Gravity (for intermittent feedings) May not be appropriate for thicker formulas made with real food ingredients or blenderized formulas.
- Feeding Pump (for continuous feeding and some intermittent feedings).
A feeding method (the timing and delivery) may be chosen because of:
- The type and location of the feeding tube you have
- The reason you need the tube feeding
- How often you need tube feeding
- How you manage your tube feeding at home
Syringe Feeding
Uses a large syringe to deliver the formula. The formula can be gently pushed into your feeding tube using the syringe plunger or it can flow from the syringe into your feeding tube using gravity.
Gravity Feeding
Uses a feeding bag and tubing which you hang on a pole above the level of your stomach. Gravity will move the formula from the bag through the tubing and into your feeding tube.
Feeding Pump
A special device that controls the timing and amount of formula given. Formula flows from a feeding bag or pre-filled container through tubing that runs into the pump and then into your feeding tube.
Common Types of Feeding Tubes
There are several different locations where a feeding tube may be placed. Each of these locations allows the nutrients in the formula to be used by your body just as if you were eating a regular meal.
NJ-tube (nasojenjunal)
This feeding tube passes through the nose, throat and esophagus, continues through the stomach, and ends in the second section of your small intestine.
J-Tube (jejunostomy)
This tube is inserted through the abdominal wall directly into the jejunum, which is the second section of your small intestine.
NG-tube (nasogastric)
This feeding tube passes through the nose, throat and esophagus and ends in your stomach.
G-tube (gastrostomy tube)
This feeding tube is inserted through the abdominal wall directly into your stomach.
NJ-tube (nasojenjunal)
This feeding tube passes through the nose, throat and esophagus, continues through the stomach, and ends in the second section of your small intestine.
J-Tube (jejunostomy)
This tube is inserted through the abdominal wall directly into the jejunum, which is the second section of your small intestine.
NG-tube (nasogastric)
This feeding tube passes through the nose, throat and esophagus and ends in your stomach.
G-tube (gastrostomy tube)
This feeding tube is inserted through the abdominal wall directly into your stomach.
Administration Methods & Guidance
Syringe Feeding
Syringe Feeding Supplies:
- Formula
- Clean measuring cup with pour spout (optional)
- 60 mL syringe*
- Water (lukewarm)
Setting Up Syringe Feeding:
- Wash your hands thoroughly with soap and water.
- Wipe the top of the formula container with clean, wet paper towel.
- Mix the formula well by shaking or mixing as directed.
- Pour formula into a clean measuring cup (or directly into the syringe once attached to your feeding tube or feeding tube extension).
Starting the Syringe Feeding:
- To administer the feeding, sit or lie with your head elevated at least 30 degrees. (about the height of two pillows) and remain in this position for 30 to 60 minutes after each feeding.
- Open (uncap) your feeding tube or feeding tube extension and attach syringe and gently flush with 30 mL of lukewarm water or the amount directed by your healthcare professional and close (recap) feeding tube or feeding tube extension.
- Remove plunger from the syringe.
- Pinch, clamp, or fold over your feeding tube or feeding tube extension to stop the flow of any fluid. Open (uncap) feeding tube or feeding tube extension and reattach the syringe.
- Fill syringe with the prescribed amount of formula and release (unpinch/unclamp/unfold) feeding tube or feeding tube extension to allow formula to flow by gravity into your stomach.
- Raise or lower the height of the syringe to increase or decrease the feeding rate. If you prefer to control the flow of your formula you can leave the plunger in the syringe, draw up your formula, and slowly push on the top of the plunger to force formula into your feeding tube.
- If indicated, add more formula to the syringe until you have received your full prescribed amount and close (recap) your feeding tube or feeding tube extension.
- After feeding is complete, replace the plunger into the syringe and draw up 30 mL of lukewarm water or the amount directed by your healthcare professional. Open (uncap) the feeding tube or feeding tube extension and reattach the syringe and flush feeding tube.
- Detach the syringe from the feeding tube or feeding tube extension and close (recap) the feeding tube.
- Clean, rinse, and dry your equipment after each feeding.
- Replace your syringes as directed by your home care supplier.
Pump Feeding
Pump Feeding Supplies:
- Pump
- Formula
- 60 mL syringe*
- Feeding container and tubing (pump set)
- Pole or feeding pump backpack
- Water (lukewarm)
Setting Up Pump Feeding:
- Wash your hands thoroughly with soap and water.
- Wipe the top of the formula container with clean, wet paper towel.
- Mix the formula well by shaking or mixing as directed.
- Pour formula into feeding container and close cap. To reduce the risk of bacterial contamination, fill your feeding container with just enough formula for up to 8 hours. If you are using powdered formula, fill your feeding container with enough formula for up to 4 hours.
- Hang the feeding container on the pole above the feeding pump or place securely inside the backpack.
- If you are using a pre-filled feeding bag, shake the bag and connect to the pump set as directed and continue from this step.
- Since every pump is different, follow the instructions provided by your healthcare professional to set up and operate your pump.
Starting the Pump Feeding:
- To administer the feeding, sit or lie with your head elevated at least 30 degrees (about the height of two pillows) and remain in this position for 30 to 60 minutes after the feeding.
- Prime your feeding pump and set flow rate on pump as directed to the recommended mL per hour.
- Open (uncap) your feeding tube or feeding tube extension.
- Before starting the feeding, use the syringe to flush your feeding tube with 30 mL of lukewarm water or the amount directed by your healthcare professional.
- Connect the end of the pump set tubing to your feeding tube or feeding tube extension.
- If applicable, open the clamp or roller clamp on the pump set tubing.
- Start your pump to begin infusing the formula.
- If additional formula is needed for hang times >8 hours, rinse out the feeding bag and tubing with lukewarm water before adding fresh formula. Refill your feeding bag again with just enough formula for up to 8 hours, 4 hours if using a powdered formula.
- After the feeding, disconnect the pump set tubing from your feeding tube or feeding tube extension. Recap the end of the tubing with the plastic cap.
- Using the syringe, flush your feeding tube again with 30 mL of lukewarm water or the amount directed by your healthcare professional.
- Close (recap) your feeding tube or feeding tube extension.
- Don’t forget to rinse before refilling your feeding container with formula (at least every 8 hours).
- If using a pre-filled bag of formula, throw it away when empty or no later than 48 hours after starting the feeding.
- Replace your feeding bag, tubing and syringes as directed by your home care supplier.
Gravity Feeding
Gravity Feeding Supplies:
- Feeding bag/container
- Formula
- 60 mL syringe*
- Tubing (gravity set)
- Pole
- Water (lukewarm)
Setting Up Gravity Feeding:
- Wash your hands thoroughly with soap and water.
- Wipe the top of the formula container with clean, wet paper towel.
- Mix the formula well by shaking or mixing as directed.
- Fill the feeding container with the number of mL or containers of formula, and close as instructed.
- Hang the feeding container on the pole so it is at least 18 inches above the level of your stomach.
- If using a pre-filled feeding bag, shake the bag and connect to the gravity set as directed and continue from this step.
- Open the clamp on the flow regulator until the formula flows towards the end of the tubing to approximately ¼ to ½ inch above the connector to avoid spilling formula into the moat of the ENFit® connector.
- Close the clamp on the flow regulator.
- Make sure the drip chamber is approximately half full.
Starting the Gravity Feeding:
- To administer the feeding, sit or lie with your head elevated at least 30 degrees (or about the height of two pillows) and remain in this position 30 to 60 minutes after the feeding.
- Open (unclamp or uncap) your feeding tube or feeding tube extension.
- Before starting the feeding, use the syringe to flush your feeding tube with 30 mL of lukewarm water or the amount directed by your healthcare professional.
- Connect the end of the gravity set tubing to your feeding tube or feeding tube extension (unclamp feeding tube or feeding tube extension if applicable).
- Open the flow regulator clamp to adjust the flow rate to the number of drops or mL per minute, as instructed. Or slowly adjust the roller clamp up or down to increase or decrease the flow of formula.
- The time each feeding takes will depend on the rate and the amount of feeding.
- After the feeding, close and disconnect the feeding set.
- Using the syringe, flush your feeding tube again with 30 mL of lukewarm water or the amount directed by your healthcare professional.
- Close (reclamp or recap) your feeding tube or feeding tube extension.
- Rinse the feeding container, tubing and syringe with warm water after each feeding and let dry.
- If using a pre-filled bag of formula, throw it away when empty or no later than 48 hours after starting the feeding.
- Replace your gravity set container with tubing and syringes as directed by your home care supplier.
* Or appropriate size syringe directed by your healthcare professional.
ENFit® is a registered trademark of GEDSA.
Personal Care
Your Mouth
Regardless of the type and location of your feeding tube, it’s important to maintain good oral health. The following steps are recommended to keep your mouth as clean as possible. Follow any other special instructions from your healthcare professionals.
Download the Tube-Feeding Personal Care Checklist here.- Brush your teeth, gums and tongue at least two times a day using a soft toothbrush and toothpaste.
- To moisten your mouth, use oral swabs, ice chips or sugar-free chewing gum.
- Freshen your mouth and breath by using mouthwash. For children, check with your healthcare professional.
- To moisten your lips, use lip balm or a lanolin-based moisturizing cream. To prevent chapping, avoid licking your lips.
- Report bleeding or anything unusual in your mouth to your healthcare professional.
Your Tube Site
If you have a gastrostomy or jejunostomy tube, care of the skin surrounding the feeding site is very important.
Follow these steps:
- Wash your hands thoroughly with soap and water.
- Remove the old dressing and tape, being careful not to disturb the tube.
- Cleanse the skin around the tube daily with soap and water as directed by your healthcare professional.
- To remove any crusting around the tube site, use cotton swabs moistened with warm water.
- Check the tube site every day for signs of redness, soreness, swelling or unusual drainage. Report anything unusual to your healthcare professional.
- Dry the skin around the feeding tube site thoroughly. Healed gastrostomy or jejunostomy sites usually do not need a special dressing. If you have been told to apply a dressing, follow the instructions from your healthcare professional.
Your Nose
If you are receiving your feeding through a nasogastric or nasointestinal tube, the tube passing through your nose may cause mild soreness or you may notice some thick, crusty mucus in your nostrils.
It is important to take care of your nose.
Follow these steps:
- On a daily basis, change the tape holding your tube in place.
- When retaping, allow some slack so that the tube does not rub against your nostrils.
- Clean your nostrils at least once a day with a soft washcloth or cotton swabs moistened with warm water.
- Remove sticky tape residue with a special adhesive remover.
- Remove crusting on the nostril with warm water on a cotton swab.
- Apply a lip balm or lanolin-based moisturizing cream to the inside edges of the nostril.
- Report any redness, bleeding or numbness to your healthcare professional.
How to Give Medication Using a Syringe
Water is part of your formula, but extra water and sometimes medications are needed to keep your body healthy and your feeding tube working properly.
Your healthcare professional will tell you how much water or medication to take.
Crush medications into fine particles or use liquid medications when available. Check with your nurse, doctor or pharmacist to get specific instructions on:
- How to crush medications
- How much water to mix with your medication
- Which medications should not be crushed
- Medications that need special considerations when given through a feeding tube

When administering water and medications, follow all the steps below:
- Do NOT add medication directly to your tube feeding formula, unless specifically directed to by your healthcare professional.
- Avoid mixing medications together during administration. Administer each medication separately.
- Using a 20 mL or larger syringe*, flush your feeding tube with at least 15 mL of lukewarm water before administering medication (unless instructed otherwise by your healthcare professional). Do not force the water flush. If you have difficulty flushing your feeding tube, contact your healthcare professional.
- Using a 20 mL or larger syringe*, draw up correct dose of medication or water for flushing into syringe. Open your feeding tube or feeding tube extension and connect the syringe to your feeding tube or feeding extension.
- Gently push the water and medication into the feeding tube or feeding tube extension.
- Remove the syringe from your feeding tube or feeding tube extension and refill the syringe with at least 15 mL of lukewarm water or the amount directed by your healthcare professional to flush after the medication.
- Repeat each step with each medication, always rinsing your syringe between medications.
- Flush a final time with at least 15 mL of lukewarm water. (unless instructed otherwise by your healthcare professional).
- Close (recap) your feeding tube or feeding tube extension when finished and place the cap back on the end of the syringe.
* Or appropriate size syringe directed by your healthcare professional.
Printable Quick Start Guides


Learn how to take medications through your feeding tube.
View / Print

Learn how to feed yourself through your tube.
View / PrintTalk with your healthcare professional to see if a Nestlé Health Science formula is right for you. The content on this website is for educational purposes only and should not be considered to be medical advice. It is not intended to replace the advice of your healthcare team. Please consult your healthcare team with any questions about the appropiate nutition and delivery of you or your child's nutrition.